Summary
Fractures of the distal femur are rare and severe. The estimated frequency is 0.4% with an epidemiology that varies: there is a classic bimodal distribution, with a frequency peak for men in their 30s and a peak for elderly women; however, at present it is found predominantly in women and in the elderly with more than 50% of patients who are over 65. The most common mechanism is an indirect trauma on a bent knee, and more rarely direct trauma by crushing. The anatomy of the distal femur explains the three major types of fracture. Because of the anatomy of the distal femur, only surgical treatment is indicated to stabilize the fracture. A non-surgical treatment is a rare option. The aim of this report was to provide an update on the existing surgical solutions for the management of these fractures and describe details of the surgical technique applicable to these injuries. Recent radiological, clinical and biomechanical data published in the literature are reported to compare different surgical options.
Fractures of the distal femur are rare and severe. The estimated frequency is 0.4% with an epidemiology that varies: there is a classic bimodal distribution, with a frequency peak for men in their 30s and a peak for elderly women; however, at present it is found predominantly in women and in the elderly with more than 50% of patients who are over 65. The most common mechanism is an indirect trauma on a bent knee, and more rarely direct trauma by crushing. The anatomy of the distal femur explains the three major types of fracture. Because of the anatomy of the distal femur, only surgical treatment is indicated to stabilize the fracture. A non-surgical treatment is a rare option. The aim of this report was to provide an update on the existing surgical solutions for the management of these fractures and describe details of the surgical technique applicable to these injuries. Recent radiological, clinical and biomechanical data published in the literature are reported to compare different surgical options.
Keywords
Distal femur, Fracture, Supracondylar and intercondylar fracture, Internal fixation, Biomechanics
Introduction
Fractures of the distal femur are rare and severe. The estimated frequency is 0.4% of all fractures and 3% of femoral fractures [1]. A classic bimodal distribution is found with a peak in frequency in young men (in their 30s) and elderly women (in their 70s). The usual context is a high energy trauma in a young patient and a domestic accident in an elderly person [1]. The gender ratio has changed and today there is a majority of women (1 man/2 women), and the population is also increasingly older; mean 61 years old at fracture and over 65 in more than half the cases [1]. Sufficient stabilization to withstand static loading forces on bone and dynamic muscular forces can only be obtained with surgery. An orthopedic treatment is rare: it is proposed in bedridden patients and/or in patients with reduced autonomy in fractures with little or no displacement.
The goal of this study was to provide an update on the management of these fractures. The basic points of treatment are summarized. The technical details and the indications of the different surgical treatments are then described. Finally, recent radiological, clinical and biomechanical results published in the literature are reported to compare the techniques.
Management and therapeutic principles
Initial management
Besides a clinical examination and a standard radiological examination, a CT scan is recommended because 55% of these fractures are intra-articular [1]. If there is a doubt about the presence of vascular injury, appropriate tests should be performed. It should be remembered that the presence of a distal pulse does not exclude vascular injury. Femoral nerve block is indicated and recommended by same authors in the emergency room [2]. These fractures are serious with a high mortality rate in elderly populations which is comparable to that found in the proximal femur. It has been shown that a delay in surgery by more than 4 days (whatever the cause) is associated with an increase in mortality at 6 and 12 months of follow-up [3]. The known risk factors are dementia as well as cardiac and kidney disorders [3]. To reduce perioperative morbidity and mortality in this age group, Kammerlander et al. [4] advise appropriate initial medical management and taking measures to prevent complications that may compromise functional results. In a series of 43 patients in their 80s, they reported 50% mortality at the 5-year follow-up, a frequent loss of independence, and only 18% of patients who can walk without help.
The major principles of treatment
Fractures of the distal femur are severe and medical management and treatment are difficult. The 1988 SOFCOT symposium reported [5]: infection and septic nonunion in 13% (29% of open fractures), aseptic nonunion in 14%, residual stiffness in 35%, secondary post-traumatic osteoarthritis in 50%, with initial chondral injury as well as incomplete reduction.
The main therapeutic principles are as follows. If the fracture is intra-articular, joint reconstruction is the first step. The knee must remain free and mobile at the surgical site. Exposure of epiphyseal fracture lines is obtained with the knee bent, especially with frontal lines. Stabilization on the frontal plane is usually not difficult, while saggital plane stability with rotation of the condyles is much more difficult. The metaphyseal portion, in particular of the anterior cortex can serve as a reference point. The second step includes reducing the epiphysis on the metaphyso-diaphysis: this is performed with the leg in extension. In case of a comminutive fracture, rotation and length should be carefully controlled.
Surgical options
For an extra-articular fracture, all therapeutic options are possible and mini-invasive surgery can be performed. In case of an intra-articular fracture, open reduction and internal plate fixation should be performed with the patient on a standard operating table.
External fixation
External fixation is not indicated for definitive treatment of these fractures, in particular in displaced intra-articular fractures. It is difficult to control alignment, the stability of this technique is poor (lever arm of the leg), there is no fixation of the articular component and stabilization of the fracture requires bridging the knee, which increases the risk of stiffness. The indications are more often for temporary fixation. If there is a complex fracture, the fracture can be evaluated and a therapeutic strategy can be determined using this solution. A bilateral fracture or a floating knee are typical examples of these complex fractures (Fig. 1). External fixation provides medical management and a Damage Orthopedic Control approach which reduces pain and facilitates treatment. Local monitoring of an open fracture is facilitated. Finally, in case of associated vascular injury, the fracture must be stabilized rapidly.
Distal femur, Fracture, Supracondylar and intercondylar fracture, Internal fixation, Biomechanics
Introduction
Fractures of the distal femur are rare and severe. The estimated frequency is 0.4% of all fractures and 3% of femoral fractures [1]. A classic bimodal distribution is found with a peak in frequency in young men (in their 30s) and elderly women (in their 70s). The usual context is a high energy trauma in a young patient and a domestic accident in an elderly person [1]. The gender ratio has changed and today there is a majority of women (1 man/2 women), and the population is also increasingly older; mean 61 years old at fracture and over 65 in more than half the cases [1]. Sufficient stabilization to withstand static loading forces on bone and dynamic muscular forces can only be obtained with surgery. An orthopedic treatment is rare: it is proposed in bedridden patients and/or in patients with reduced autonomy in fractures with little or no displacement.
The goal of this study was to provide an update on the management of these fractures. The basic points of treatment are summarized. The technical details and the indications of the different surgical treatments are then described. Finally, recent radiological, clinical and biomechanical results published in the literature are reported to compare the techniques.
Management and therapeutic principles
Initial management
Besides a clinical examination and a standard radiological examination, a CT scan is recommended because 55% of these fractures are intra-articular [1]. If there is a doubt about the presence of vascular injury, appropriate tests should be performed. It should be remembered that the presence of a distal pulse does not exclude vascular injury. Femoral nerve block is indicated and recommended by same authors in the emergency room [2]. These fractures are serious with a high mortality rate in elderly populations which is comparable to that found in the proximal femur. It has been shown that a delay in surgery by more than 4 days (whatever the cause) is associated with an increase in mortality at 6 and 12 months of follow-up [3]. The known risk factors are dementia as well as cardiac and kidney disorders [3]. To reduce perioperative morbidity and mortality in this age group, Kammerlander et al. [4] advise appropriate initial medical management and taking measures to prevent complications that may compromise functional results. In a series of 43 patients in their 80s, they reported 50% mortality at the 5-year follow-up, a frequent loss of independence, and only 18% of patients who can walk without help.
The major principles of treatment
Fractures of the distal femur are severe and medical management and treatment are difficult. The 1988 SOFCOT symposium reported [5]: infection and septic nonunion in 13% (29% of open fractures), aseptic nonunion in 14%, residual stiffness in 35%, secondary post-traumatic osteoarthritis in 50%, with initial chondral injury as well as incomplete reduction.
The main therapeutic principles are as follows. If the fracture is intra-articular, joint reconstruction is the first step. The knee must remain free and mobile at the surgical site. Exposure of epiphyseal fracture lines is obtained with the knee bent, especially with frontal lines. Stabilization on the frontal plane is usually not difficult, while saggital plane stability with rotation of the condyles is much more difficult. The metaphyseal portion, in particular of the anterior cortex can serve as a reference point. The second step includes reducing the epiphysis on the metaphyso-diaphysis: this is performed with the leg in extension. In case of a comminutive fracture, rotation and length should be carefully controlled.
Surgical options
For an extra-articular fracture, all therapeutic options are possible and mini-invasive surgery can be performed. In case of an intra-articular fracture, open reduction and internal plate fixation should be performed with the patient on a standard operating table.
External fixation
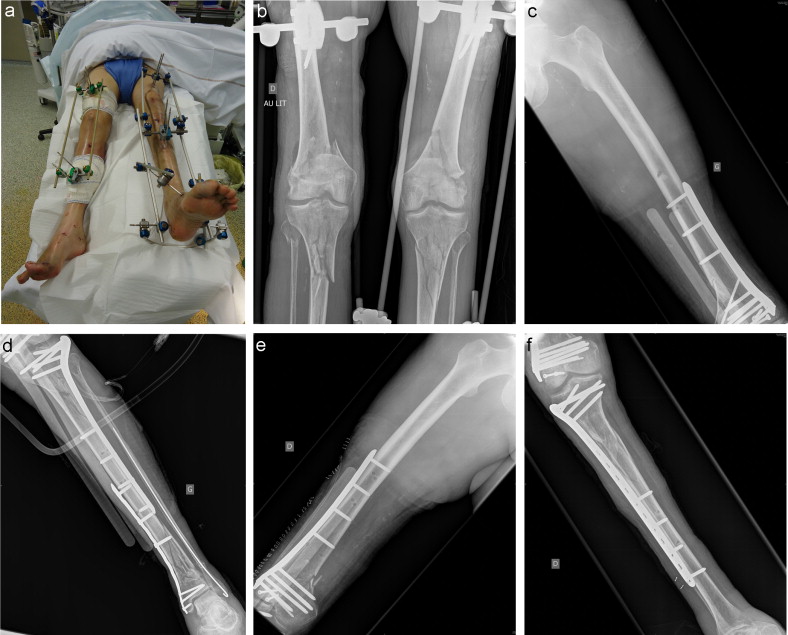
External fixation is not indicated for definitive treatment of these fractures, in particular in displaced intra-articular fractures. It is difficult to control alignment, the stability of this technique is poor (lever arm of the leg), there is no fixation of the articular component and stabilization of the fracture requires bridging the knee, which increases the risk of stiffness. The indications are more often for temporary fixation. If there is a complex fracture, the fracture can be evaluated and a therapeutic strategy can be determined using this solution. A bilateral fracture or a floating knee are typical examples of these complex fractures (Fig. 1). External fixation provides medical management and a Damage Orthopedic Control approach which reduces pain and facilitates treatment. Local monitoring of an open fracture is facilitated. Finally, in case of associated vascular injury, the fracture must be stabilized rapidly.

External fixation should bridge the knee when there is intra-articular involvement. The femoral pins should be at a distance from the fracture site and the joint to prevent infection. Anterior femoral pins can be a good choice if internal fixation with a lateral plate is used later: in that case external fixation is maintained during the procedure to facilitate control of alignment during internal fixation. Although temporary external fixation has certain advantages, there are still certain risks. Control of the fracture is limited, and there is a risk of skin damage from a protruding bone fragment. Oh et al. [6] reported results of a series of 59 complex intra-articular fractures with temporary bridging external fixation. There were seven complications including four that developed in distal femoral fractures. The authors explain this rate of infection and the unsuccessful control of length that occurred by the abundant femoral leg muscles and the presence of the suprapatellar pouch. On the other hand, Parekh et al. [7] reported good results in the two-step management of complex intra-articular fractures around the knee (with 16 distal femoral fractures in a series of 47 cases). Finally, Bonnevialle et al. [8] reported a series of 27 fractures of the femoral diaphysis and 26 fractures of the distal femur treated with a lateral external monoplane fixator with a high rate of infection and knee stiffening in the “distal fracture” group. They concluded that definitive external fixation is only indicated in stable distal metaphyseal-diaphyseal fractures when the epiphysis has first been stabilized.
Anterograde intramedullary nailing
The indications for anterograde intramedullary nailing are essentially extra-articular fractures. Certain intra-articular fractures without or with very little displacement can be treated with this technique as long as the epiphyseal part of the fracture has been stabilized with isolated screws to avoid opening of the fracture site during nailing. Finally, in the rare cases of bi- or trifocal fractures of the distal femur, nailing is often the only therapeutic alternative (Fig. 2). This solution is contraindicated in complex intra-articular fractures.

The advantages of this technique are that it is closed with conservation of heamatoma and that the implant is extra-articular which is relatively easy to remove. The patient should be installed on a traction table. If condylar traction is being performed (extra-articular fracture), this should be as anterior as possible. If there is intra-articular involvement, a traction boot is indicated. Recurvatum deformity of the distal fragment is controlled by providing distal support attached to the traction table (Fig. 3). Additional internal fixation of an epiphyseal fragment should take into account the position of the future nail. The nail should descend as deeply as possible into the condyle for maximum stability. Antekeier et al. [9] defined the minimum distance between the fracture site and the most proximal screw for distal fixation of the nail. Anterograde intramedullary nailing is possible when the fracture is located more than 3 cm from the proximal screw, which can resist one million cycles of loading. The diameter of the nail is also important. For Huang et al. [10], distal cortical contact increases stability of the system while reducing strains which are absorbed by the nail and the locking screws.

Retrograde nailing
The indications for retrograde nailing are classic: extra-articular fracture, simple intra-articular fractures with little or no displacement. This technique may be indicated in cases of floating knee with a single surgical approach for stabilization of both fracture sites.
Passing a nail near the fractured trochlea can worsen the situation by opening the fracture site, thus if there is an intra-articular fracture line, initial screw fixation is indicated. Retrograde nailing has the advantages of being a closed technique, but because it is intra-articular, there is a risk of septic arthritis in case of infection. Removal is also more difficult. The patient can be installed on a standard or a fracture table. On a standard table, the knee is in 30° flexion and the distal femur is supported. On a fracture table, reduction is obtained by skeletal traction at the proximal tibia with the leg hanging slightly. The nail should be inserted deep enough to avoid any impingement with the patella and should not be used as a lever to prevent creating an intercondylar fracture line. Epiphyseal fixation can be improved by using a screw and counter screw.
Simple screw fixation
Simple screw fixation is proposed in the presence of a frontal or sagittal unicondylar fracture.
A medial or lateral parapatellar approach is often necessary, however, in case of a fracture with no or little displacement, a percutaneous procedure is possible and reduction is controlled by ligamentotaxis. A recent study showed that osteosynthesis using two 6.5 mm screws were more effective than osteosynthesis using two or four 3.5 mm screws [11]. A load of 40–56% more was required with 6.5 mm screws to cause system failure. In frontal fractures, the direction of the screws changes the mechanical stability. Double screws using cancellous lag screws in a posterior to anterior direction provide better mechanical strength during loading than those in an anterior to posterior direction [12].
Blade plate
Classic indications are extra-articular fractures, sagittal unicondylar fractures or supracondylar and intercondylar fractures.
This is a monoblock, preshaped implant that is adapted to the anatomy of the distal femur. The system is very stable allowing compression of the epiphyseal-metaphyseal fracture site. In osteoporotic bone, placement of the blade can be traumatic and have little resistance to breakage. Mechanically, the plate functions like a dynamic tension band and creates medial compression. The 95° blade plate is placed on a femur whose articular surface is in 1–3° valgus. In this way, the difference in angle between the plate and the distal end of the femur results in medial compression of the metaphyseal fracture site after diaphyseal fixation, thanks to the deformation of the blade plate. For an optimal effect, the medial pillar must be perfectly reconstructed. The diaphyseal position of the plate is determined by the position of the blade which must be precisely defined. It should be located 2 cm from the joint line (AP and lateral view), along the axis of the femoral diaphysis and in the middle of the anterior half of the largest diameter of the condyle in profile. Thus the blade is inserted in front of the Blumensatt line (avoiding the cruciate ligaments) and behind the groove of the trochlea (avoiding the patellofemoral joint line). The path is perpendicular to the lateral cortex, aimed approximately a dozen degrees towards the back to prevent internal rotation and medial translation of the distal fragment. The blade should not extend beyond the medial cortex to prevent injuries of the medial collateral ligament.
Dynamic compression plate
The indications are classic: extra-articular fractures, sagittal unicondylar fractures or supra- and intercondylar fractures.
This solution includes dynamic epiphyseal screw fixation (lag screw) for compression of the fracture site. Epiphyseal fixation is obtained by a single screw which the plate pivots upon for sagittal adjustment. The 95° angle between the plate and the screw facilitates frontal placement and positions the ephiphyseal screw parallel to the joint. This system has the advantage of being fairly easy to position, because the screw is cannulated, to limit bone trauma and to have good resistance to screw failure. However the screw hole is large, there may be rotational instability in the distal screw before diaphyseal fixation and the insertion site of the screw may be located near a frontal fracture. The insertion guide is positioned according to the same criteria as the blade plate, and its direction on the axial plane is parallel to the anterior trochlear rims, or 10° downwards and inwards.
Locking compression plate
The classic indications are extra-articular fractures, sagittal unicondylar fractures or supra- and intercondylar fractures.
The goal of locking plate is to provide better stability in fragile bone. Primary stability of the plate is independent of the friction effect as the screw presses the plate, and is obtained by locking the screw into the plate. Plate design is usually anatomical which allows it to be used as a “reduction mold”, molding the bone to the plate.
The locking plate can be used during an open procedure when there is intra-articular involvement, or with mini-invasive surgery using the ancillary less invasive stabilization system (LISS) in case of an extra-articular fracture or in the presence of a simple non- displaced fracture [13]. Combination use is possible, with mini-invasive proximal diaphyseal fixation combined with open distal internal fixation. Mini-invasive surgery reduces postoperative pain, and facilitates functional recovery [14]. Its main disadvantage is the lack of epiphyseal compression with locking screws, requiring prior placement of standard additional screws. These screws should not interfere with the plate. The rules for fixation of this system must be strictly followed, in particular during mini-invasive surgery to prevent malunion and mechanical failure [15]. The patient can be installed according to the surgeon's preference. If the patient is installed on a traction table, traction should be moderate and a certain degree of impaction of the fragments should be preserved, especially in elderly patients to promote union. The first step of the mini-invasive surgery is to mark the skin with references (fracture, joint line, patella, femoral stems of an existing implant, femoral axis, incision) which will help reduce the amount of radiation to the patient, choose the length of the plate and facilitate the procedure. The lateral paracondylar approach is used. The length of the plate is chosen to leave at least five holes above the fracture. The goal is to obtain coverage that is as long as possible to absorb and distribute strains and stresses. It is necessary to remain extra-articular by raising the suprapatellar pouch. The beveled tip of the plate allows minimally traumatic submuscular and extraperiosteal insertion. The plate should be parallel to the lateral cortex in front, centered on the femoral diaphysis in profile, with the racket of the distal femoral plate located behind the base of the trochlea and in front of the Blumensatt line. The anatomical plate can be used as a reduction mold if and only if the plate is, firstly, parallel to the lateral cortex of the femur (parallel to the cortex does not mean in contact with bone), secondly, the epiphyseal screws are parallel to the joint line. The second part of the procedure includes placing a 2 mm pin along the path of the central screw of the LISS system which should be parallel to the joint line. The bone can then be pulled towards the plate with a traction screw or by using the LISS system. To obtain a perfect reduction, different technical tricks can be used (lag screw from the bone to the plate, temporary intrafocal pinning, temporary screws, joystick pin) [13], [14], [15].
Numerous biomechanical studies have been performed to evaluate and define locking plate fixation systems. The LCP® (Synthes, Etupes, France) system is usually the reference and is compared to classic internal fixation systems. Dougherty et al. [16] suggest that bicortical screws should be systematically used to provide three points of fixation (2 cortical + the plate) to limit breakage. The position of the screw in relation to the fracture line depends on the type of fracture. If the fracture is unstable (long fracture line, comminutive fracture) locking screws are placed near the fracture line to stabilize the fracture site. If it is a simple fracture, locking screws are placed further away with an open hole on each side of the fracture to create elasticity in the system, which will promote union [17]. For Ahmad et al. [18], the internal fixation system should be close to the fracture. A distance of less than 2 mm provides better resistance to compression and torsion, while there is significant plastic deformity with more than 5 mm. LCP plates have combination screw holes making it possible to use a “locked system”, a dynamic compression plate (DCP) system or a “combination” system. Stoeffel et al. [19] compared these three systems. The locking system results in less loss of reduction under axial compression with less plastic deformity and the DCP system provides better strength under torsion. The authors propose combination fixation. Bottlang et al. [20] propose the use of a standard screw at the end of the plate in case of a fracture in osteoporotic bone to limit strains and prevent a stress fracture. This type of system increases strength during bending without changing strength under compression or torsion. The implant must be parallel at a 10° angle to the cortex and the lateral condyle. Indeed Khalafi et al. [21] have shown that these parallel systems are stronger under axial compression and cyclic loading than systems in which the plate is not parallel to the lateral cortex. Beingessner et al. [22] compared “titanium” plates to steel plates as well as unicortical to bicortial screws in these indications. They showed that strength under torsion is reduced in “titanium” plates and strength is improved with bicortical screws. On the other hand, there is no difference for axial compression strains and plastic deformity. Lujan et al. [23] concluded that “titanium” plates favor the formation of calluses by increasing elasticity in fixation material. Finally, for Wilkens et al. [24], the placement of polyaxial screws increases strength under axial compression and torsion and reduces deformation observed under cyclic loading.
Total knee arthroplasty
As in complex fractures of the proximal humerus, the distal humerus and fractures of the femoral neck, total knee arthroplasties can be included as a therapeutic option in elderly patients.
This is a difficult procedure in a fragile population requiring extensive expertise in arthroplasty. The main technical point is to restore the height of the joint line when there is no longer any possibility of reduction. An intact lateral or medial pillar facilitates adjustment of the replacements. A constrained knee replacement is usually chosen and even in certain cases a megaprosthesis such as that used after tumor resection. Postoperative morbidity-mortality is high. In a series of 54 fractures in patients in their 80s, Appleton et al. [25] reported a mortality of 40% and a morbidity of 15% at 1 year with 11% of surgical revisions and 4% of implant revisions. Patient selection is essential to guarantee the best results. Finally, certain authors propose a hinged prosthesis to treat nonunion of the distal femur in elderly patients. After a mean follow-up of 4 years in a series of 10 patients mean age 74 years old, Vaishya et al. [26] reported satisfactory functional results with a very low morbidity in eight patients. Haidukewych et al. [27] proposed a total knee replacement for nonunion of the distal femur as well as for early failure of internal fixation. Survival was 91%, after 5 years in 15 patients with perioperative complications in 29%, postoperative complications in 29%, and poorer results than for primary replacements.
Results in the literature
Biomechanical data
Several biomechanical studies have shown that locking systems are better than classic internal fixation (DCP plate, retrograde nailing, blade plate) [28], [29], [30]. Fulkerson et al. [28] compared locking plates to classic large fragment plates with cables. Strength under axial compression and torsion was increased in locking plates, however failures were more severe with opening of the proximal femoral fragment. Zlowodzki et al. [29] compared LCP, blade plates, and retrograde nailing in extra-articular fractures. Strength under axial compression was better with the LCP system than with the blade plate or nailing, by 34 and 13% respectively, but strength under torsion was reduced. The authors observed better distal fixation with the LCP system with loss of distal fixation in only one LCP plate (6%), three blade plates (38%) and eight losses with retrograde intramedullary nailing (100%). These same authors compared the blade plate to the LCP system in cadavers with high bone density and did not find any significant difference in compression strength [30]. Finally, Hingins et al. [31] concluded that the locking plate system was better than the blade plate with increased strength under axial compression and cyclic loading whatever the quality of cadaveric bone. To our knowledge, no studies have been performed to compare anteretrograde intramedullary nailing to locking plates. Overall, biomechanical results showed that locking plates are better.
Clinical results
Vallier and Immler [32] compared the 95° blade plate and LCP locking plates in a retrospective series of 71 intra-articular and extra-articular fractures. The rates of complications, surgical revisions and nonunion were statistically higher with LCP plates. On the other hand, Nayak et al. [33] support the use of LCP locking plates for extra-articular fractures, reporting union in all cases, good recovery of alignment and high quality function. An autologous graft was not necessary with the mini-invasive technique, postoperative pain was reduced and the rate of union was high. Kolb et al. [34] confirmed these results in a retrospective series of 50 fractures. Functional recovery was found to be very good with 80% of good and very good results. They concluded that the locking plate system allows early mobility, rapid functional recovery and good radiological results with low morbidity, even though these were intra-articular fractures. Kanabar et al. [35] and Kavali et al. [36] proposed fixation of complex fractures of the distal femur with locking plates by mini-invasive approach emphasizing the limited blood loss and low rate of complications. Kavali et al. [36] did not find any statistical difference in functional recovery between patients treated for single or multiple fractures. Comparisons in the literature between retrograde intramedullary nailing and blade plate by a mini-invasive approach have not shown any difference between intra-articular or extra-articular fractures. Markmiller et al. [37] did not report improved results for any particular implant for identical indications. Hierholzer et al. [38] confirmed these results in a retrospective series of 115 fractures comparing retrograde nailing (n = 59) and mini-invasive locking plate (n = 56). The authors describe the indications for each technique: the plate can be adapted to all fractures, while retrograde nailing is better adapted to extra-articular fractures. They emphasize that high quality results are more dependent upon the surgical technique than the choice of implant. On the other hand, results comparing retrograde nailing and classic open internal fixation are clear. For Thompson et al. [39], statistical results for the rate of surgical revision and the rate of malunion are better for retrograde intramedullary nailing. The rates of infection and nonunion were higher in the open internal fixation group. After a mean follow-up of 6 years nearly 50% of intra-articular fractures showed progression to arthritis on radiological imaging. Acharya et Rao [40] reported a prospective series in 28 patients treated with retrograde nailing with union in 93%, malunion in 14% and excellent or good functional results in 75% of cases. There was no difference between results for retro- and anteretrograde nailing. For Salem et al. [41], results in length, torsion, alignment and function were comparable. The only reported difference was in hip range of motion which was more limited with anteretrograde intramedullary nailing, and knee range of motion which was more limited with retrograde nailing. Hartin et al. [42] did not observe any difference in functional recovery in a randomized comparison of the treatment of extra-articular fractures by retrograde intramedullary nailing and blade plate. The only element observed was more frequent pain in the knee in the retrograde nailing group, so that fixation material had to be removed in 25% of the cases. The results in the literature do not provide any consensus on the technique – only closed techniques seem to make a difference. It is important to remember that the best results are obtained with techniques in which the surgeon has the most experience.
Conclusion
The quality of the surgical technique is the primary factor, and the only guarantee of obtaining good radiological and clinical results in distal femoral fractures. Mini-invasive treatment (nailing or plates) seems to provide better results. All types of fractures can be treated with locking plates and a classic or mini-invasive surgical approach is possible. Although the overall mid-term results are satisfactory, there are no studies evaluating the long-term functional and radiological results of fractures of the distal femur. However, there seems to be a tendency towards progression to arthritis in intra-articular fractures. Recent biomechanical studies have shown that results are better with locking plates. The surgical technique must be rigorous and the biomechanical qualities of these implants must be understood to prevent the development of major complications.

Leave A Comment